Screening and Treating Malnutrition in Community Care Settings
Malnutrition is a major clinical and public health problem in the UK. It’s estimated that over 3 million people are malnourished, with 93% living in the community and 1.3 million aged over 65 (1).
A person is classified as malnourished if they meet a set of criteria which often includes a low Body Mass Index (BMI), significant and unintentional weight loss over a defined period of time, and/or reduced nutritional intake over a defined period of time (2).
In community care settings, NICE guidelines recommend that nutritional screening for malnutrition is conducted on admission to care homes and when there is a clinical concern (3). Screening is a rapid and simple way to detect those with or at risk of malnutrition so that suitable action plans can be implemented.
However, recent evidence (4) suggests that nutritional screening is not being fully implemented. Failure to screen or inaccurate scoring could lead to missed nutritional intervention which could have serious consequences for patients. Additionally, the Care Quality Commission (CQC) can prosecute health and social care providers who fail to conduct adequate nutritional needs assessments if it results in avoidable harm or risk of harm to a person using the service (5). Therefore, it’s important that all staff involved with nutrition-risk screening are suitably trained to meet the required standards for their organisation.
The Malnutrition Universal Screening Tool (MUST) is the most frequently used in the UK. It’s a five-step tool which is suitable for screening adults across all care settings. It’s a scoring system that uses objective or subjective measurements to establish nutrition risk. Patients are deemed to be either low, medium, or high risk of malnutrition. For more information on how to conduct MUST screening, click here.
A food-first approach is a simple way of providing enhanced nutrition to those who are or at risk of becoming malnourished. It can be useful for patients who still have a good appetite. Fortifying foods help to increase the nutritional density of the diet without increasing the volume of food consumed.
Several foods which can be used to fortify the diet include: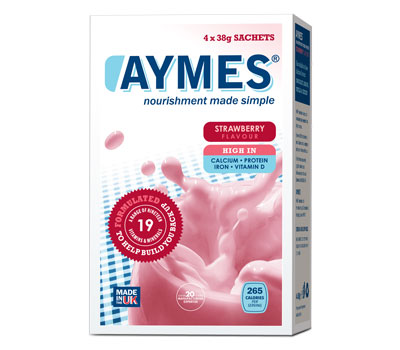
○ Double Cream
○ Full Fat Milk
○ Honey/Syrup/Sugar
○ Butter
○ Cheese
○ Milk Powder
○ Oils such as olive oil
Additional snacks can be used to improve nutritional intake and examples include cakes, biscuits, crisps, cheese and crackers, and custard. Encouraging patients to consume nourishing drinks that provide more energy and protein than tea, coffee or water is also an effective strategy.
AYMES Retail is a nutritionally-balanced, milkshake-style drink designed to help give an additional boost to those who do not require a medical prescription. It provides up to 266 calories per serving when mixed with 200ml whole milk. It’s presented conveniently in individual cartons containing 4 x 38g sachets and comes in a variety of flavours (chocolate, strawberry, banana, vanilla) to help prevent flavour fatigue. With an RRP of just £3.19, it is available to buy at pharmacies and via the AYMES website.
By Harriet Smith, Registered Dietitian





